Macular Degeneration
Perhaps you have just learned that you or a loved one has age-related macular degeneration, also known as AMD. If you are like many people, you probably do not know a lot about the condition or understand what is going on inside your eyes.
This page will give you a general overview of AMD. You will learn about the following:
- Risk factors and symptoms of AMD
- Treatment options
- Low vision services that help people make the most of their remaining eyesight
- Support groups and others who can help
The aim is to answer your questions and to help relieve some of the anxiety you may be feeling.
What is AMD?
AMD is a common eye condition and a leading cause of vision loss among people age 50 and older. It causes damage to the macula, a small spot near the center of the retina and the part of the eye needed for sharp, central vision, which lets us see objects that are straight ahead.
In some people, AMD advances so slowly that vision loss does not occur for a long time. In others, the disease progresses faster and may lead to a loss of vision in one or both eyes. As AMD progresses, a blurred area near the center of vision is a common symptom. Over time, the blurred area may grow larger or you may develop blank spots in your central vision. Objects also may not appear to be as bright as they used to be.
AMD by itself does not lead to complete blindness, with no ability to see. However, the loss of central vision in AMD can interfere with simple everyday activities, such as the ability to see faces, drive, read, write, or do close work, such as cooking or fixing things around the house.
The Macula
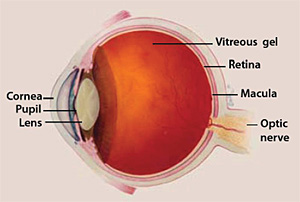
The macula is made up of millions of light-sensing cells that provide sharp, central vision. It is the most sensitive part of the retina, which is located at the back of the eye. The retina turns light into electrical signals and then sends these electrical signals through the optic nerve to the brain, where they are translated into the images we see. When the macula is damaged, the center of your field of view may appear blurry, distorted, or dark.
Who is at risk?
Age is a major risk factor for AMD. The disease is most likely to occur after age 60, but it can occur earlier. Other risk factors for AMD include:
- Smoking. Research shows that smoking doubles the risk of AMD.
- Race. AMD is more common among Caucasians than among African-Americans or Hispanics/Latinos.
- Family history. People with a family history of AMD are at higher risk.
Does lifestyle make a difference?
Researchers have found links between AMD and some lifestyle choices, such as smoking. You might be able to reduce your risk of AMD or slow its progression by making these healthy choices:
- Avoid smoking
- Exercise regularly
- Maintain normal blood pressure and cholesterol levels
- Eat a healthy diet rich in green, leafy vegetables and fish
How is AMD detected?
The early and intermediate stages of AMD usually start without symptoms. Only a comprehensive dilated eye exam can detect AMD. The eye exam may include the following:
- Visual acuity test. This eye chart measures how well you see at distances.
- Dilated eye exam. Your eye care professional places drops in your eyes to widen or dilate the pupils. This provides a better view of the back of your eye. Using a special magnifying lens, he or she then looks at your retina and optic nerve for signs of AMD and other eye problems.
- Amsler grid. Your eye care professional also may ask you to look at an Amsler grid. Changes in your central vision may cause the lines in the grid to disappear or appear wavy, a sign of AMD.
- Fluorescein angiogram. In this test, which is performed by an ophthalmologist, a fluorescent dye is injected into your arm. Pictures are taken as the dye passes through the blood vessels in your eye. This makes it possible to see leaking blood vessels, which occur in a severe, rapidly progressive type of AMD (see below). In rare cases, complications to the injection can arise, from nausea to more severe allergic reactions.
- Optical coherence tomography. You have probably heard of ultrasound, which uses sound waves to capture images of living tissues. OCT is similar except that it uses light waves, and can achieve very high-resolution images of any tissues that can be penetrated by light—such as the eyes. After your eyes are dilated, you’ll be asked to place your head on a chin rest and hold still for several seconds while the images are obtained. The light beam is painless.
During the exam, your eye care professional will look for drusen, which are yellow deposits beneath the retina. Most people develop some very small drusen as a normal part of aging. The presence of medium-to-large drusen may indicate that you have AMD.
Another sign of AMD is the appearance of pigmentary changes under the retina. In addition to the pigmented cells in the iris (the colored part of the eye), there are pigmented cells beneath the retina. As these cells break down and release their pigment, your eye care professional may see dark clumps of released pigment and later, areas that are less pigmented. These changes will not affect your eye color.
Questions to ask your eye care Professional
Below are a few questions you may want to ask your eye care professional to help you understand your diagnosis and treatment. If you do not understand your eye care professional's responses, ask questions until you do understand.
- What is my diagnosis and how do you spell the name of the condition?
- Can my AMD be treated?
- How will this condition affect my vision now and in the future?
- What symptoms should I watch for and how should I notify you if they occur?
- Should I make lifestyle changes?
What are the stages of AMD?
There are three stages of AMD defined in part by the size and number of drusen under the retina. It is possible to have AMD in one eye only, or to have one eye with a later stage of AMD than the other.
- Early AMD. Early AMD is diagnosed by the presence of medium-sized drusen, which are about the width of an average human hair. People with early AMD typically do not have vision loss.
- Intermediate AMD. People with intermediate AMD typically have large drusen, pigment changes in the retina, or both. Again, these changes can only be detected during an eye exam. Intermediate AMD may cause some vision loss, but most people will not experience any symptoms.
- Late AMD. In addition to drusen,
people with late AMD have vision loss from damage to the macula. There are two types of late AMD:
- In geographic atrophy (also called dry AMD), there is a gradual breakdown of the light-sensitive cells in the macula that convey visual information to the brain, and of the supporting tissue beneath the macula. These changes cause vision loss.
- In neovascular AMD (also called wet AMD), abnormal blood vessels grow underneath the retina. ("Neovascular" literally means "new vessels.") These vessels can leak fluid and blood, which may lead to swelling and damage of the macula. The damage may be rapid and severe, unlike the more gradual course of geographic atrophy. It is possible to have both geographic atrophy and neovascular AMD in the same eye, and either condition can appear first.
AMD has few symptoms in the early stages, so it is important to have your eyes examined regularly. If you are at risk for AMD because of age, family history, lifestyle, or some combination of these factors, you should not wait to experience changes in vision before getting checked for AMD.
Not everyone with early AMD will develop late AMD. For people who have early AMD in one eye and no signs of AMD in the other eye, about five percent will develop advanced AMD after 10 years. For people who have early AMD in both eyes, about 14 percent will develop late AMD in at least one eye after 10 years. With prompt detection of AMD, there are steps you can take to further reduce your risk of vision loss from late AMD.
If you have late AMD in one eye only, you may not notice any changes in your overall vision. With the other eye seeing clearly, you may still be able to drive, read, and see fine details. However, having late AMD in one eye means you are at increased risk for late AMD in your other eye. If you notice distortion or blurred vision, even if it doesn’t have much effect on your daily life, consult an eye care professional.
Early AMD
Currently, no treatment exists for early AMD, which in many people shows no symptoms or loss of vision. Your eye care professional may recommend that you get a comprehensive dilated eye exam at least once a year. The exam will help determine if your condition is advancing.
As for prevention, AMD occurs less often in people who exercise, avoid smoking, and eat nutritious foods including green leafy vegetables and fish. If you already have AMD, adopting some of these habits may help you keep your vision longer.
Intermediate and late AMD
Researchers at the National Eye Institute tested whether taking nutritional supplements could protect against AMD in the Age-Related Eye Disease Studies (AREDS and AREDS2). They found that daily intake of certain high-dose vitamins and minerals can slow progression of the disease in people who have intermediate AMD, and those who have late AMD in one eye.
The first AREDS trial showed that a combination of vitamin C, vitamin E, beta-carotene, zinc, and copper can reduce the risk of late AMD by 25 percent. The AREDS2 trial tested whether this formulation could be improved by adding lutein, zeaxanthin or omega-3 fatty acids. Omega-3 fatty acids are nutrients enriched in fish oils. Lutein, zeaxanthin and beta-carotene all belong to the same family of vitamins, and are abundant in green leafy vegetables.
The AREDS2 trial found that adding lutein and zeaxanthin or omega-three fatty acids to the original AREDS formulation (with beta-carotene) had no overall effect on the risk of late AMD. However, the trial also found that replacing beta-carotene with a 5-to-1 mixture of lutein and zeaxanthin may help further reduce the risk of late AMD. Moreover, while beta-carotene has been linked to an increased risk of lung cancer in current and former smokers, lutein and zeaxanthin appear to be safe regardless of smoking status.
Here are the clinically effective doses tested in AREDS and AREDS2:
- 500 milligrams (mg) of vitamin C
- 400 international units of vitamin E
- 80 mg zinc as zinc oxide (25 mg in AREDS2)
- 2 mg copper as cupric oxide
- 15 mg beta-carotene, OR 10 mg lutein and 2 mg zeaxanthin
A number of manufacturers offer nutritional supplements that were formulated based on these studies. The label may refer to "AREDS" or "AREDS2."
If you have intermediate or late AMD, you might benefit from taking such supplements. But first, be sure to review and compare the labels. Many of the supplements have different ingredients, or different doses, from those tested in the AREDS trials. Also, consult your doctor or eye care professional about which supplement, if any, is right for you. For example, if you smoke regularly, or used to, your doctor may recommend that you avoid supplements containing beta-carotene.
Even if you take a daily multivitamin, you should consider taking an AREDS supplement if you are at risk for late AMD. The formulations tested in the AREDS trials contain much higher doses of vitamins and minerals than what is found in multivitamins. Tell your doctor or eye care professional about any multivitamins you are taking when you are discussing possible AREDS formulations.
Finally, remember that the AREDS formulation is not a cure. It does not help people with early AMD, and will not restore vision already lost from AMD. But it may delay the onset of late AMD. It also may help slow vision loss in people who already have late AMD.
Advanced neovascular AMD
Neovascular AMD typically results in severe vision loss. However, eye care professionals can try different therapies to stop further vision loss. You should remember that the therapies described below are not a cure. The condition may progress even with treatment.
- Injections. One option to slow the progression of neovascular AMD is to inject drugs into the eye. With neovascular AMD, abnormally high levels of vascular endothelial growth factor (VEGF) are secreted in your eyes. VEGF is a protein that promotes the growth of new abnormal blood vessels. Anti-VEGF injection therapy blocks this growth. If you get this treatment, you may need multiple monthly injections. Before each injection, your eye will be numbed and cleaned with antiseptics. To further reduce the risk of infection, you may be prescribed antibiotic drops. A few different anti-VEGF drugs are available. They vary in cost and in how often they need to be injected, so you may wish to discuss these issues with your eye care professional.
- Photodynamic therapy. This technique involves laser treatment of select areas of the retina. First, a drug called verteporfin will be injected into a vein in your arm. The drug travels through the blood vessels in your body, and is absorbed by new, growing blood vessels. Your eye care professional then shines a laser beam into your eye to activate the drug in the new abnormal blood vessels, while sparing normal ones. Once activated, the drug closes off the new blood vessels, slows their growth, and slows the rate of vision loss. This procedure is less common than anti-VEGF injections, and is often used in combination with them for specific types of neovascular AMD.
- Laser surgery. Eye care professionals treat certain cases of neovascular AMD with laser surgery, though this is less common than other treatments. It involves aiming an intense "hot" laser at the abnormal blood vessels in your eyes to destroy them. This laser is not the same one used in photodynamic therapy which may be referred to as a "cold" laser. This treatment is more likely to be used when blood vessel growth is limited to a compact area in your eye, away from the center of the macula, that can be easily targeted with the laser. Even so, laser treatment also may destroy some surrounding healthy tissue. This often results in a small blind spot where the laser has scarred the retina. In some cases, vision immediately after the surgery may be worse than it was before. But the surgery may also help prevent more severe vision loss from occurring years later.
Questions to ask your eye care professional about treatment
- What is the treatment for advanced neovascular AMD?
- When will treatment start and how long will it last?
- What are the benefits of this treatment and how successful is it?
- What are the risks and side effects associated with this treatment and how has this information been gathered?
- Should I avoid certain foods, drugs, or activities while I am undergoing treatment?
- Are other treatments available?
- When should I follow up after treatment?
Loss of Vision
Coping with AMD and vision loss can be a traumatic experience. This is especially true if you have just begun to lose your vision or have low vision. Having low vision means that even with regular glasses, contact lenses, medicine, or surgery, you find everyday tasks difficult to do. Reading the mail, shopping, cooking, and writing can all seem challenging.
However, help is available. You may not be able to restore your vision, but low vision services can help you make the most of what is remaining. You can continue enjoying friends, family, hobbies, and other interests just as you always have. The key is to not delay use of these services.
What is vision rehabilitation?
To cope with vision loss, you must first have an excellent support team. This team should include you, your primary eye care professional, and an optometrist or ophthalmologist specializing in low vision. Occupational therapists, orientation and mobility specialists, certified low vision therapists, counselors, and social workers are also available to help. Together, the low vision team can help you make the most of your remaining vision and maintain your independence.
Second, talk with your eye care professional about your vision problems. Ask about vision rehabilitation, even if your eye care professional says that "nothing more can be done for your vision." Vision rehabilitation programs offer a wide range of services, including training for magnifying and adaptive devices, ways to complete daily living skills safely and independently, guidance on modifying your home, and information on where to locate resources and support to help you cope with your vision loss.
What are some low vision devices?
Because low vision varies from person to person, specialists have different tools to help patients deal with vision loss. They include:
- Reading glasses with high-powered lenses
- Handheld magnifiers
- Video magnifiers
- Computers with large-print and speech-output systems
- Large-print reading materials
- Talking watches, clocks, and calculators
- Computer aids and other technologies, such as a closed-circuit television, which uses a camera and television to enlarge printed text
Keep in mind that low vision aids without proper diagnosis, evaluation, and training may not work for you. It is important that you work closely with your low vision team to get the best device or combination of aids to help improve your ability to see.
Questions to ask your eye care professional about low vision
- How can I continue my normal, routine activities?
- Are there resources to help me?
- Will any special devices help me with reading, cooking, or fixing things around the house?
- What training is available to me?
- Where can I find individual or group support to cope with my vision loss?
Charles Bonnet syndrome (Visual Hallucinations)
People with impaired vision sometimes see things that are not there, called visual hallucinations. They may see simple patterns of colors or shapes, or detailed pictures of people, animals, buildings, or landscapes. Sometimes these images fit logically into a visual scene, but they often do not.
This condition can be alarming, but don’t worry—it is not a sign of mental illness. It is called Charles Bonnet syndrome, and it is similar to what happens to some people who have lost an arm or leg. Even though the limb is gone, these people still feel their toes or fingers or experience itching. Similarly, when the brain loses input from the eyes, it may fill the void by generating visual images on its own.
Charles Bonnet syndrome is a common side effect of vision loss in people with AMD. However, it often goes away a year to 18 months after it begins. In the meantime, there are things you can do to reduce hallucinations. Many people find the hallucinations occur more frequently in evening or dim light. Turning on a light or television may help. It may also help to blink, close your eyes, or focus on a real object for a few moments.
Coping with AMD
AMD and vision loss can profoundly affect your life. This is especially true if you lose your vision rapidly.
Even if you experience gradual vision loss, you may not be able to live your life the way you used to. You may need to cut back on working, volunteering, and recreational activities. Your relationships may change, and you may need more help from family and friends than you are used to. These changes can lead to feelings of loss, lowered self-esteem, isolation, and depression.
In addition to getting medical treatment for AMD, there are things you can do to cope:
- Learn more about your vision loss.
- Visit a specialist in low vision and get devices and learning skills to help you with the tasks of everyday living.
- Try to stay positive. People who remain hopeful say they are better able to cope with AMD and vision loss.
- Stay engaged with family and friends.
- Seek a professional counselor or support group. Your doctor or eye care professional may be able to refer you to one.
Information for family members
Shock, disbelief, depression, and anger are common reactions among people who are diagnosed with AMD. These feelings can subside after a few days or weeks, or they may last longer. This can be upsetting to family members and caregivers who are trying to be as caring and supportive as possible.
Following are some ideas family members might consider:
- Obtain as much information as possible about AMD and how it affects sight. Share the information with the person who has AMD.
- Find support groups and other resources within the community.
- Encourage family and friends to visit and support the person with AMD.
- Allow for grieving. This is a natural process.
- Lend support by "being there."
Education Navigation
- Monday: 9:00AM - 6:00PM
- Tuesday: 9:00AM - 6:00PM
- Wednesday: 9:00AM - 6:00PM
- Thursday: 9:00AM - 6:00PM
- Friday: 9:00AM - 2:00PM
- Saturday: CLOSED
- Sunday: CLOSED
